The World Health Organization (WHO) defines self-care as “the ability of individuals, families, and communities to promote health, prevent disease, maintain health, and cope with illness and disability with or without the support of a healthcare provider.”
The concept of self-care is not new; however, rapid advancement in medical and digital technologies is accelerating the range of interventions that can be acquired and managed more directly by individuals. Such “self-care interventions” offer self-directed, convenient, and quality health care that can contribute to universal health coverage.
On June 24, 2019, the WHO released the Consolidated Guideline on Self-Care Interventions for Health: Sexual and Reproductive Health and Rights (SRHR) stating, “self-care interventions are among the most promising and exciting new approaches to improve health and well-being, both from a health systems perspective and for people who use these interventions.” The consolidated guideline calls for the adoption of national guidelines and includes people-centered, evidence-based recommendations for key self-care interventions for SRHR such as HIV self-testing, human papillomavirus self-sampling, and self-administered injectable contraception. The COVID-19 crisis has created a greater urgency to advance self-care work in order to offer continuity of SRHR services in low physical touch environments. On June 1, 2020, the WHO endorsed self-care approaches as a part of its COVID-19 Operational Guidance.
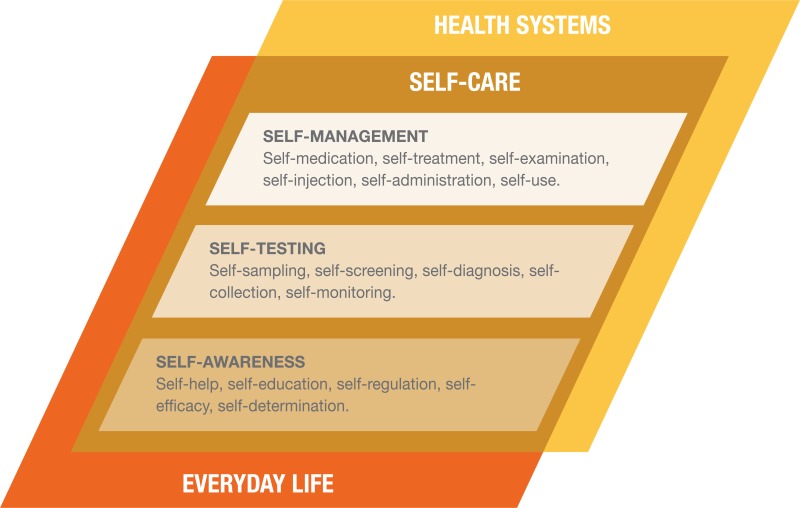
Image above: Self-care in the context of interventions linked to health systems, from WHO Consolidated Guideline on Self-Care Interventions for Health
In this Trending Topic, we provide a selection of tools and project examples on the topic of self-care, and we welcome our readers to upload their own materials on this topic.
Banner Image: U.S. Ambassador Ted Osius and his spouse Clayton Bond join Vietnamese government officials and celebrities to demonstrate how to do the HIV self-test. Ho Chi Minh City, August 26, 2016. Photo: Phuong Nguyen/USAID. Retrieved from https://www.flickr.com/photos/49951534@N08/29129213082 on July 14, 2020.




