In Kenya, maternal health complications are a leading cause of morbidity among women. Kenya’s Rift Valley Province has consistently had the highest level of abortion-related outpatient morbidity in the country since at least 2003. These realities necessitate interventions to prevent unintended or mistimed pregnancies and to ensure access to quality care for women with postabortion complications
The RESPOND Project designed an intervention package aimed at increasing awareness and use of postabortion care (PAC) services and improving family planning, reproductive health, and maternal health outcomes. Known as the Community Mobilization for Postabortion Care (COMMPAC) intervention, this package builds on efforts by The ACQUIRE Project (2005–2007) to address PAC and increase family planning (FP) uptake by focusing on the central role that communities can play in improving access to services.
Community mobilization that fosters engagement through local participation is a popular mechanism to improve the planning for and use of health care in resource-limited settings. Such mobilization can raise awareness of when health care is necessary, where effective care is available, and how to seek timely care, and it can leverage community resources,which—in addition to having the potential to reduce the stigma associated with PAC—ultimately improves well-being and responsiveness to health problems.
RESPOND worked with districts and communities to: strengthen service delivery points to provide PAC services; conduct community mobilization to improve community members’ involvement in and knowledge about the prevention and treatment of postabortion complications; build communities’ capacity to address needs related to PAC; and encourage those most marginalized and most affected by postabortion complications to engage in community action to improve the situation.
The stated goal of the project was to Increase communities‘ awareness and use of postabortion care (PAC) and related services to reduce maternal mortality and morbidity by:
- Increasing community knowledge of the danger signs of abortion-related complications, locations of services, and FP–related information and services
- Building capacity to address PAC and FP needs
- Encouraging involvement of the marginalized in community action
- Mobilizing communities to prevent and treat incomplete abortion
- Strengthening service delivery points providing PAC and FP
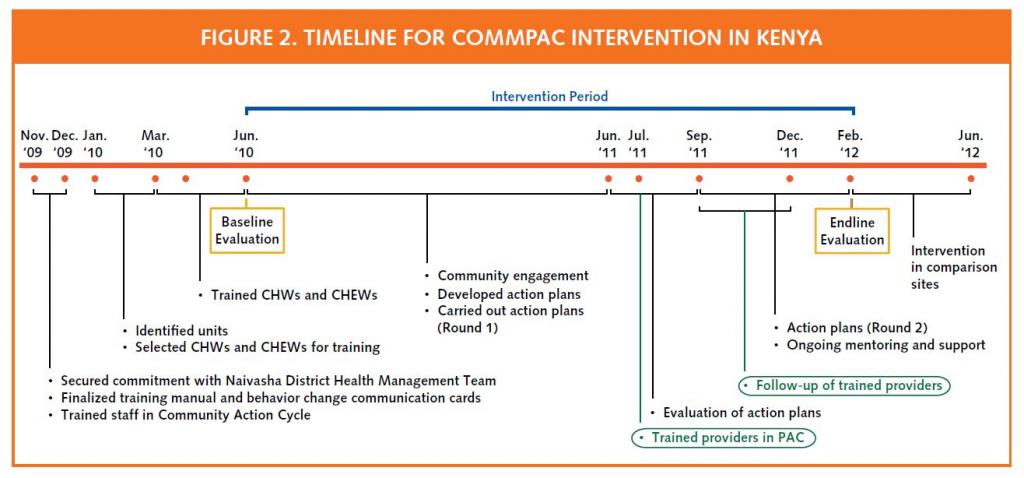
TIMELINE of the Project (click on image to see larger version)
Sources:
- Communities Take Action in Kenya: Strengthening Postabortion Care
- Community mobilization and service strengthening to increase awareness and use of postabortion care and family planning in Kenya (article in the International Journal of Obstetrics and Gynecology, July 26, 2014 pp 8-13)
Timeline
Inquire
A baseline data collection exercise was carried out from May to June 2010 in Naivasha District to provide a benchmark against which the RESPOND intervention may be measured during endline evaluation. The evaluation used a quasi-experimental design with intervention and control groups covering six study sites within Naivasha District, with measurements taken at baseline and endline. The baseline data collection comprised three components
- A community-based survey of approximately 600 women between the ages of 18 and 49
- An inventory of all public and private health facilities in the study area (n=11
- Interviews with providers working at the identified facilities
Results included the following
- There is a clear need for PAC services at the evaluation sites
- Utilization of health services during pregnancy and delivery is limited
- Knowledge of FP is high, but actual use is significantly lower
- Reasons for nonuse of FP highlight the need for the intervention
- Exposure to community interventions in general is low
- Health facilities in Naivasha could feasibly offer PAC services
- Government health facilities are patronized by a considerable proportion of women

Design the Strategy
The MOH Community Strategy was the foundation for enhancing the accountability and responsibility of service providers and community members alike and for increasing access to, and use of, sustainable, decentralized, lower-level healthcare services in the community units.
The project was designed as an 18 month intervention as follows:
- MOH Community Strategy w/District Health Management Teams (DHMTs)
- Community Health Extension Workers (CHEWs) and Community Health Workers (CHWs) as primary links—sustainable structures
- Facilitated Community Action Cycle for PAC
- Trained CHEWs/CHWs
- Supported them to conduct community mobilization
- Support groups to develop and implement action plans
- Mentoring to build capacity of CHEWs/CHWs
- Trained providers in comprehensive PAC services
- Built provider-community partnerships
Community Action Cycle – The Community Action Cycle is a highly participatory process in which community members learn how to take action for their own health.

Create and Test
A set of community behavior change communication flip cards was created for the CHEWs and CHWs to use in house-to-house outreach visits and on community dialog and action days.
Topics covered included
- FP methods
- PAC
- Misconceptions and negative rumors about FP
- Danger signs
- The three delays
There was also a plan to hold community–facility linkage meetings with the trained CHEWs and CHWs to discuss progress on their action plans and to jointly resolve problems
- A Guide to Action for Community Mobilization and Empowerment Focused on Postabortion Complications
- Community Health Information Cards
Mobilize and Monitor
More than 630 community members participated in the mobilization sessions.
In addition, two community–facility linkage meetings were held with the trained CHEWs and CHWs to discuss progress on their action plans and to jointly resolve problems (including negative rumors about FP methods, religious opposition, long distances to the nearest facility, poor roads, lack of trained providers, unfavorable facility hours, lack of partner support, poor provider attitudes, and lack of equipment and supplies.
None of the local dispensaries had the capacity to provide PAC at the project’s inception.
Accordingly, in partnership with the MOH, the RESPOND Project improved the service capacity in facilities serving the communities in the intervention group. This was achieved by training 16 providers (clinical officers and nurses) at existing Naivasha dispensaries and health centers in PAC and by training 20 providers in FP. The clinical officers and nurses had received previous training in related health procedures; as part of the project, they received an additional week of PAC training and a week of FP training.
The PAC training included instruction regarding surgical procedures and manual vacuum aspiration; issues related to patient comfort, privacy, hygiene, and cleanliness in the diagnostic, waiting, and recovery areas; relevant medications, instruments, and supplies; and post-procedure counseling. The FP training included instruction on patient intake, insertion and removal of intrauterine devices and implants, and provision of oral and injectable contraceptives, and condoms. Community problem diagnosis also provided insights to the project as to how services could be refined to meet the communities’ perceived needs.
Evaluate and Evolve
The evaluation consisted of pre-post quasi-experimental design- baseline was in June 2010 and endline was in January 2012.
The control group for comparison consisted of a matched pair of three units each, with each unit containing approximately 5,000 people or five villages with two CHEWs & 50 CHWs.
The quantitative and qualitative measures were as follows:
- Community survey of 593 women aged 18–49
- Exposure to PAC community mobilization
- Sources of care: maternal and child health (MCH), PAC FP
- Perceptions of quality of care
- Use of MCH, PAC, and FP services
- Inventory and interviews with providers
- Exit interviews with PAC clients, if possible
- Monitoring data on client loads for PAC and FP services
- Focus group discussions, in-depth interviews: CHWs, CHEWs, leaders
Findings
- Increase among intervention group in hearing about FP by endline (p ≤ 0.001)
- Increased use of FP among women (intervention and comparison)
- Increase in reporting early pregnancy bleeding in intervention group from 9.8%-13.1% (p=0.14)
- Increase in intevention group seeking PAC among those who reported early pregnancy bleeding (65-80%)
- Increase in proportion of women reporting early pregnancy bleeding more than three times greater in intervention group (unadjusted p=0.005; adjusted p=0.01)
- Improvements in quality of PAC
- Reductions in waiting time at facility
- More than twice as many women in intervention group particpated in community/NGO meetings focused on PAC
- Intervention significantly increased knowledge (3.3%) of danger signs or complications
- Providers experienced increased confidence about offering PAC services
- Evaluation showed evidence of community empowerment to take action for their own health
Best Practices & Challenges
Best practices/processes/tools
- Country-led by DHMT, using MOH Community Strategy and structure
- Community engagement is important to success
- Building skills and capacity = taking action for their health
- Work with local social community networks
- Community empowerment must be combined w/quality service improvements
- Link facilities w/communities to increase use of health services throughout pregnancy
Challenges
- CHEWs/CHWs/community groups have other responsibilities
- Wide geographic coverage
- Lack of incentives; equipment and supplies
- Stigma surrounding abortion
- Insufficient time for intervention
Article about the intervention:
Community mobilization and service strengthening to increase awareness and use of postabortion care and family planning in Kenya – authors – Chi-Chi Undie, Lynn M. Van Lith, Mercy Wahome, Francis Obare, Esther Oloo, Carolyn Curtis. (International Journal of Gynaecology and Obstetrics, 2014 July (I), pp. 8-13.
Banner Photo: M. Wahome/EngenderHealth
Date of Publication: April 20, 2022

